Introduction
Vascular access is the commonest invasive procedure performed on hospitalised patients, but it is not without complications1. Complications can include phlebitis, localised infection, blood stream infection, thrombus, infiltration and extravasation, and all are preventable1.
The default vascular access device for most patients is the peripheral intravenous catheter (PIVC) that is often inserted by junior medical staff, junior nurses or in some hospitals, healthcare assistants with little assessment of the vein quality, medicines to be administered and the likely duration of treatment2. In a small study, it was found that only 5% of the nursing staff had any understanding of the pH of the intravenous medicines that were to be administered3.
There are many elderly patients in hospitals requiring vascular access, these patients often have fragile veins making cannulation difficult4. Even in the general adult patients, cannulation can pose challenges with a reported first attempt cannulation failure rate of 19%5. Once inserted, up to 50% of PIVCs fail before the completion of the intended treatment resulting in further cannulation6. Not only is this unpleasant for the patient but also involves valuable nursing and/or medical time wasting both time and resources.
The care, management and evaluation of the vascular access device is imperative to prevent complications and damage to the vein7.
Vessel Health and Preservation (VHP)
VHP is a concept first published in a paper by Nancy Moureau, Nancy Trick and colleagues in 2012 in the US where they describe the clinical pathway to select the most appropriate device for the individual patient and their treatment plan8.
The essence of the VHP concept is the ‘timely assessment, planning, insertion and ongoing assessment’ for vascular access putting the patient at the centre of the decision making8. This proactive approach moves away from the traditional reactive approach and decreases the risk of complications with an aim to improve patient experience and preserve veins for future use.
The VHP clinical pathway was adapted in the UK by a working party led by the Infection Prevention Society to develop the UK VHP Framework first published in 2016 and updated in 20209.
VHP: Four Quadrants of Care
The assessment and selection of the right vascular access device along with good care will not alone prevent all the complications. The VHP model (see figure 1) provides the 4 quadrants of care with education running through each of the quadrants7. The healthcare staff providing care within each quadrant should be suitably educated to include skill-based training and competency assessment of all the procedures they perform.
-
The first VHP Quadrant: Assessment/Selection
This quadrant describes the importance of the initial assessment to ensure the right device is selected. This includes the assessment of the patient’s medical history, comorbidities, availability of the patient’s veins, the treatment plan including duration of therapy. The device selection should select the device size based on the vein size with the aim of the smallest device accommodating the lowest number of lumens.
-
The second VHP Quadrant: Insertion and Training
This quadrant describes the importance of the inserter being suitably qualified and trained in the insertion of the vascular access device. Strict adherence to an aseptic technique is the cornerstone in preventing VAD-related infections. Maximal sterile barrier precautions are required for central VAD insertions to include sterile gloves and gown, hat and face mask and use of full-body sterile drapes. Once the device is inserted it must be secured and a sterile dressing applied. The tip of central VAD should be confirmed with either ECG technology or X-ray.
-
The third VHP Quadrant: Management
This quadrant describes the need for daily assessment to ensure that the device is still required and the most appropriate, considering any changes in diagnosis and treatment. This should identify early complications and prompt remove when the VAD is no longer required. The assessment needs to include the insertion site, functioning of the VAD, dressing and securement. An aseptic technique must be used for all access to the VAD.
-
The fourth VHP Quadrant: Evaluation
This quadrant describes the need for surveillance of complications and audits of patient outcomes. The evaluation also includes evaluation staff competency to inform educational needs and to establish a process for product evaluation.
UK Vessel Health and Preservation (VHP) Framework
The UK VHP framework was developed to support assessment and decision making for vascular access devices (VAD)9. The VHP framework was designed in a poster format with the aim to be visual and easy to follow. The first and arguably the most important question within the VHP framework is ‘genuine need for vascular access?’ prompting consideration of alternative routes for administering medication such as oral, nasal or via the rectum. These alternative routes may provide options with much lower complications.
Within the VHP framework there are four clear sections to aid the assessment and decision-making and include:
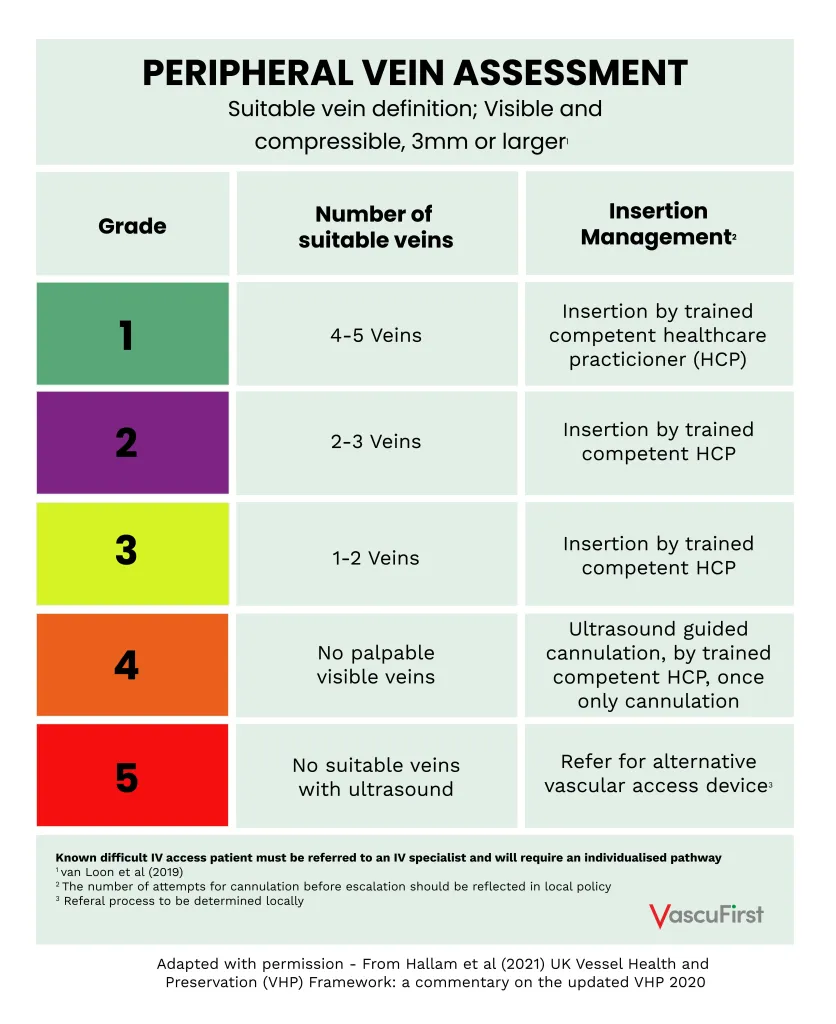
- A vein assessment tool providing a scale of 1 – 5 on the quality of peripheral veins.
- Medication suitability section for the safety of the medicines to be given with consideration of central vein administration
- A right line decision tool for device choice is based on vein quality, drug choice and duration of treatment
- An evaluation section for daily assessment of the vascular access device to observe any complications
-
The vein assessment tool
This section provides a grading of the quality of the veins (see figure 2). This helps to put some context into describing peripheral veins often just described as good or poor. This grading can empower healthcare staff to escalate early for a more skilled person to perform cannulation using ultrasound or indeed refer for an alternative device. It also recognises the need for a patient known to have difficult IV access to have a bespoke pathway.
-
Suitability of Medicines
This section highlights that all intravenous medicines potentially pose a threat to vessel health and focuses on the assessment of factors such as pH and osmolarity levels, viscosity, volume of dilution and speed of the infusion. Guidance is given to refer to the UK Medusa (Injectable Medicines Guide)10 as this has all the updated pH and osmolarity values, and to the Summary of Medicine Product Characteristics (SmPC), which is available for all medicines. Where the SmPC recommends administering an intravenous medicine via a central VAD, this should be followed.
-
The Right Line Decision Tool
The right line decision tool is presented as an algorithm which enables the clinician to combine assessments with the intended medicines, the peripheral vein condition and the duration of treatment when decision making for VAD selection. The use of ultrasound guided (USG) insertion to locate veins has been found to increase cannulation success and dwell time and reduce insertion-related complications, therefore the use of USG cannulation is included11. Where the intravenous medicine must be given via a central VAD or the peripheral vein grade doesn’t support peripheral administration, then the device choice is based on the duration of treatment.
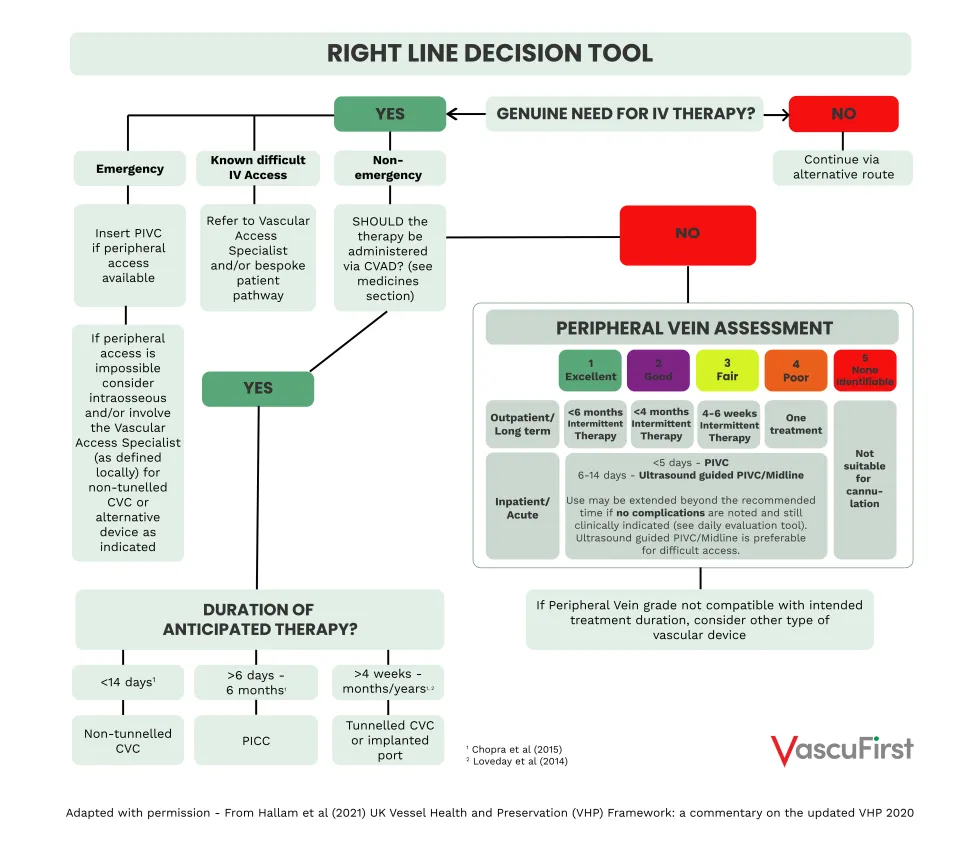
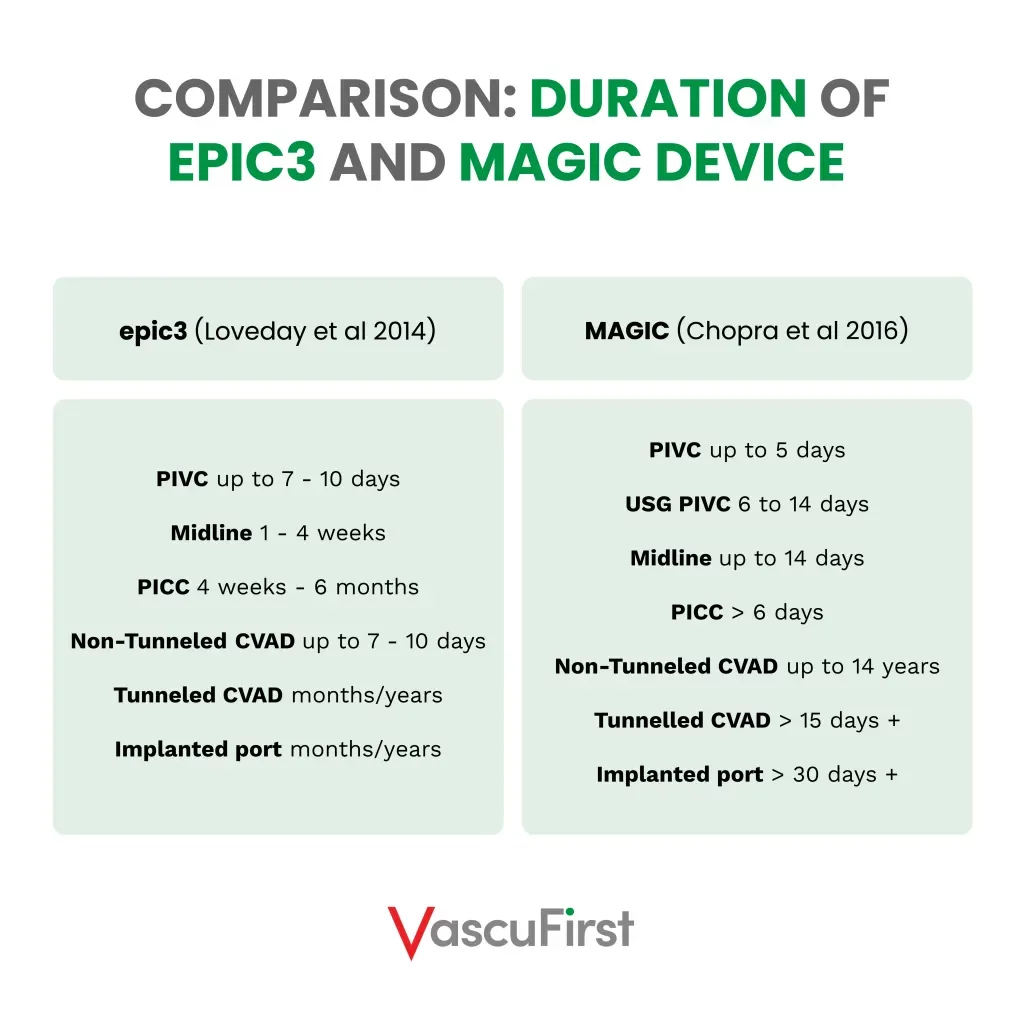
MAGIC matrix12 is used as the guide for device choice based on duration of treatment, this has altered the suggested duration of vascular access devices from the original VHP framework that was guided by the epic3 guidelines1. These changes are compared in table 1.
-
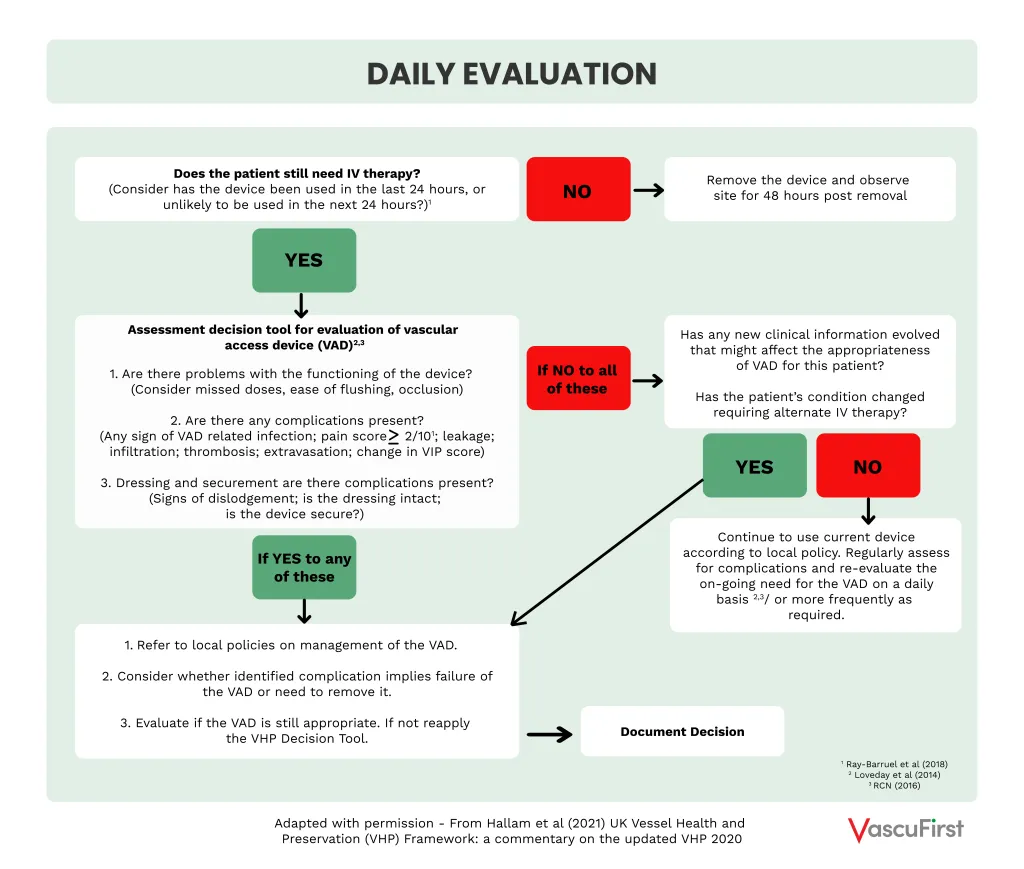
Daily evaluation
The evaluation section (see figure 4) starts with the question “does the patient still need IV therapy and has the device been used in the last 24 hours, or unlikely to be used in the next 24 hours?” to prompt timely removal of the VAD. This is followed with three questions to assess the VAD, as below:
– Are there problems with the functioning of the device?
– Are there any complications present?
– Dressing and securement; are there complications present?
A positive response to these questions may indicate that the device is not the most appropriate device to continue delivering the intended treatment for the patient and if necessary, the VHP decision tool should be reapplied. Pain has been included as a complication indicator when pain is reported as 2 or greater out of a score of 1013.
Conclusion
The VHP 4 quadrants of care provides a model to prevent complications from vascular access with the potential to improve healthcare and economic risks, improve patient experience and preserve veins for future use. The UK VHP Framework was developed using the VHP concept to assist with vascular access device selection and daily evaluation.
Further information
Further information on vessel health can be accessed from the open access book “Vessel Health and Preservation: The Right Approach to Vascular Access” https://link.springer.com/book/10.1007/978-3-030-03149-7
The UK VHP2020 resources can be accessed from the Infection Prevention Society https://www.ips.uk.net/vessel-health-and-preservation-framework-2020